A recent study published in The New England Journal of Medicine has found that tirzepatide leads to greater weight loss than semaglutide in adults with obesity, but without type 2 diabetes. The research was funded by Eli Lilly, the maker of tirzepatide.
Study Overview
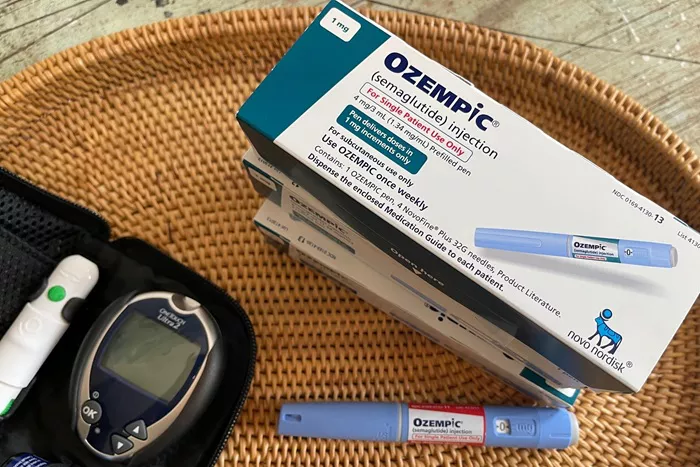
Obesity affects over 650 million adults globally, and many struggle to lose and maintain weight through lifestyle changes alone. Medications, particularly glucagon-like peptide-1 (GLP-1) receptor agonists like semaglutide, have shown promise in addressing the condition. However, a new drug called tirzepatide, which targets both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors, may offer even more significant benefits. While both drugs are approved for weight management, direct comparisons in people without diabetes have been limited.
The need to better understand the effectiveness of these medications in non-diabetic populations is crucial for making informed treatment choices. This study provides important insights into how tirzepatide and semaglutide compare for weight loss.
About the Study
This phase 3b trial enrolled 750 adults with obesity, defined by a body mass index (BMI) of 30 or higher, or 27 or higher with obesity-related complications like hypertension, sleep apnea, or cardiovascular disease. Participants were randomly assigned to receive either tirzepatide (10 mg or 15 mg) or semaglutide (1.7 mg or 2.4 mg) for 72 weeks. The study began with lower doses, gradually increasing to the maximum tolerated amounts.
All participants were also given counseling on diet and exercise, and their weight and waist measurements were regularly monitored. Safety was closely tracked, especially regarding gastrointestinal symptoms and injection-site reactions. Participants who experienced severe side effects could reduce or stop their medication, but continued to be tracked for study results.
The primary goal was to assess the percentage of body weight lost after 72 weeks. Secondary goals included tracking the percentage of participants who lost at least 10%, 15%, 20%, or 25% of their body weight, as well as changes in waist circumference.
Results
The study found that tirzepatide was significantly more effective than semaglutide at reducing body weight. On average, participants taking tirzepatide lost 20.2% of their body weight, compared to 13.7% for those on semaglutide. This difference was both statistically and clinically significant. The weight loss for tirzepatide participants equated to an average of 22.8 kg, compared to 15 kg for those taking semaglutide.
Tirzepatide was also more effective at helping participants reach key weight loss milestones. 81.6% of tirzepatide users lost at least 10% of their weight, compared to 60.5% of semaglutide users. Additionally, more people on tirzepatide achieved greater weight loss: 64.6% lost 15% of their body weight, and 48.4% lost 20%—both significantly higher percentages than those taking semaglutide.
Not only did tirzepatide result in greater weight loss, but it also showed a more significant reduction in waist circumference, with an average reduction of 18.4 cm compared to 13.0 cm in the semaglutide group.
Both medications also contributed to improvements in cardiometabolic risk factors, such as blood pressure, blood glucose, and lipid levels. These improvements were closely linked to the amount of weight lost, with those who achieved greater weight loss seeing more significant health benefits.
Interestingly, women in both groups lost about 6% more weight than men, a trend that could impact how the results are interpreted.
Safety
Both drugs were generally well tolerated. The most common side effects were gastrointestinal issues, such as nausea, diarrhea, and constipation. These were more frequent during dose adjustments and were typically mild to moderate in severity.
However, semaglutide had a higher rate of discontinuation due to these gastrointestinal side effects—5.6% compared to 2.7% for tirzepatide. On the other hand, tirzepatide was associated with a higher incidence of injection-site reactions (8.6% vs. 0.3% for semaglutide), although these did not lead to treatment discontinuation.
Overall, around 77% of participants in both groups experienced at least one adverse event, though serious events were rare (about 4% in each group). Notably, a case of pancreatitis was reported in the semaglutide group, but serious adverse events were otherwise uncommon.
Conclusion
In conclusion, the study demonstrates that tirzepatide is significantly more effective than semaglutide in helping adults with obesity (but without type 2 diabetes) lose weight. Tirzepatide not only led to greater overall weight loss but also helped a higher percentage of participants reach important weight loss milestones. It was well tolerated, with manageable side effects, and may offer significant benefits for patients with severe obesity or multiple health complications.
While the study’s open-label design could introduce some bias, the results are consistent with findings from prior blinded studies. As obesity rates continue to rise, having effective treatment options like tirzepatide will be crucial for providing personalized care that aligns with individual patient goals. This trial further supports tirzepatide’s potential to become a leading treatment for weight management and may influence future clinical guidelines and patient care decisions.