NEW YORK, May 21 (Reuters) — Cigna announced on Wednesday that it will limit out-of-pocket costs to $200 per month for patients using the weight-loss drugs Wegovy and Zepbound. This new benefit will be added to Cigna’s pharmacy benefit management plans.
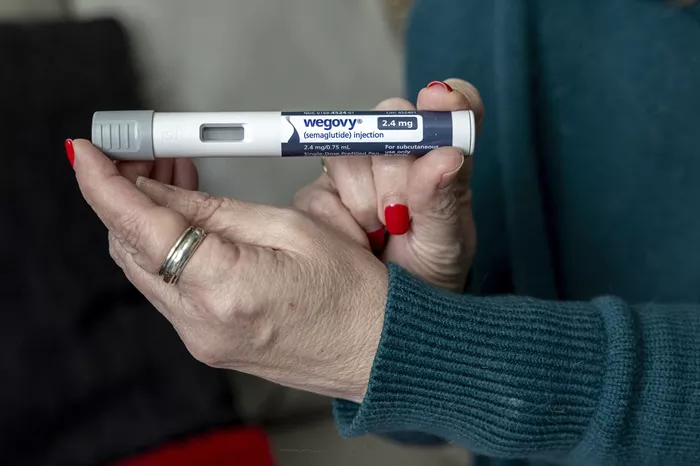
Harold Carter, senior vice president at Evernorth, said Cigna’s $200 cap is low compared to the usual cash price for these drugs. Wegovy and Zepbound, made by Novo Nordisk and Eli Lilly, have list prices close to $1,000. However, on the manufacturers’ websites, they often cost about half that or less.
The $200 co-pay will count toward a patient’s deductible. This means the amount patients pay will apply to the total they must pay before insurance covers other costs, Carter explained.
Clinical trials showed that Wegovy and Zepbound helped patients lose between 15% and 20% of their body weight. The drugs work by slowing digestion and helping users feel full longer.
While the brand-name drugs were in short supply, sales of compounded versions from companies like Hims & Hers, Noom, Weight Watchers, and Ro increased significantly.
The Food and Drug Administration (FDA) has allowed these compounded copies, but this policy will end on May 22.
Noom recently announced it plans to keep selling smaller doses of the medication even after the FDA policy ends.
A study from January found that patients without insurance paid an average of $549 to buy Zepbound directly from Eli Lilly. Patients using a discount card from Novo Nordisk paid about $650 for Wegovy.
On a different note, employees of Novo Nordisk showed support for their former CEO Lars Fruergaard Jorgensen last Friday.